Genetics Reversed
With late nights, long days and some friendly bacteria, they did it. Texas Biomed researchers developed a powerful genetics-based tool now powering COVID-19 research worldwide.

What do we need to study this novel coronavirus?
That was the question Professor Luis Martinez-Sobrido, PhD, posed to Staff Scientist Chengjin Ye, PhD, in February 2020. Dr. Martinez-Sobrido, an expert in virology, vaccines and antiviral research, had just relocated his lab and team of researchers from the University of Rochester to Texas Biomed.
“We’ll probably need reverse genetics,” Dr. Ye replied.
It was still in the very early days, before the COVID-19 pandemic was officially declared. More and more countries were reporting their first cases as SARS-CoV-2 spread around the globe. The clock was ticking to learn about the virus’s strengths and weaknesses, and develop treatments and vaccines to prevent people from dying.
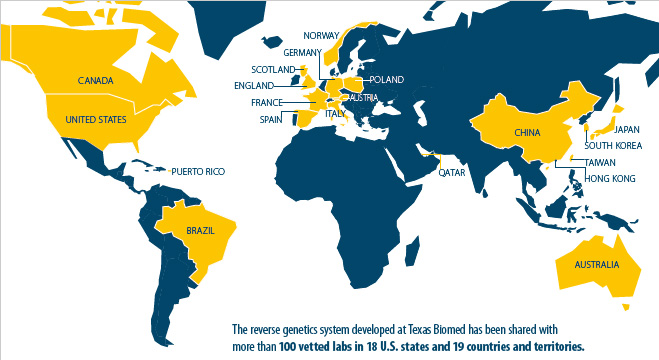
Fast forward to current day and the particular reverse genetics system developed by Dr. Martinez-Sobrido, Dr. Ye and their colleagues has drawn worldwide interest from the scientific community. Texas Biomed has shared the tool with more than 100 vetted labs across the globe, empowering more scientists as far away as Australia and Japan to advance their own COVID-19 research.
This is the fastest we’ve ever had to work. We weren’t done developing reverse genetics for one variant before the next one emerged.
Dr. Luis Martinez-Sobrido
Reverse genetics is a powerful tool. It allows researchers to systematically study the virus, to learn how it works and find ways to stop it. Specifically, it enables them to make changes to the virus’s genetic code. For example, researchers can use the system to knock out a gene to see if a virus becomes less harmful, or they can add a fluorescent marker so it is super easy to see if treatments or vaccines are working in cells and in animal models.
“Classical genetics starts with an outcome, such as hair color, and then looks for the gene responsible,” Dr. Ye says. “Reverse genetics starts with the genes and then sees what happens.”
Reverse genetics is so powerful, it must be very carefully done in regulated biosafety laboratories. It involves a multi-step process that starts with a noninfectious blueprint of the virus, and ultimately results in a version of the virus making copies of itself in cells.
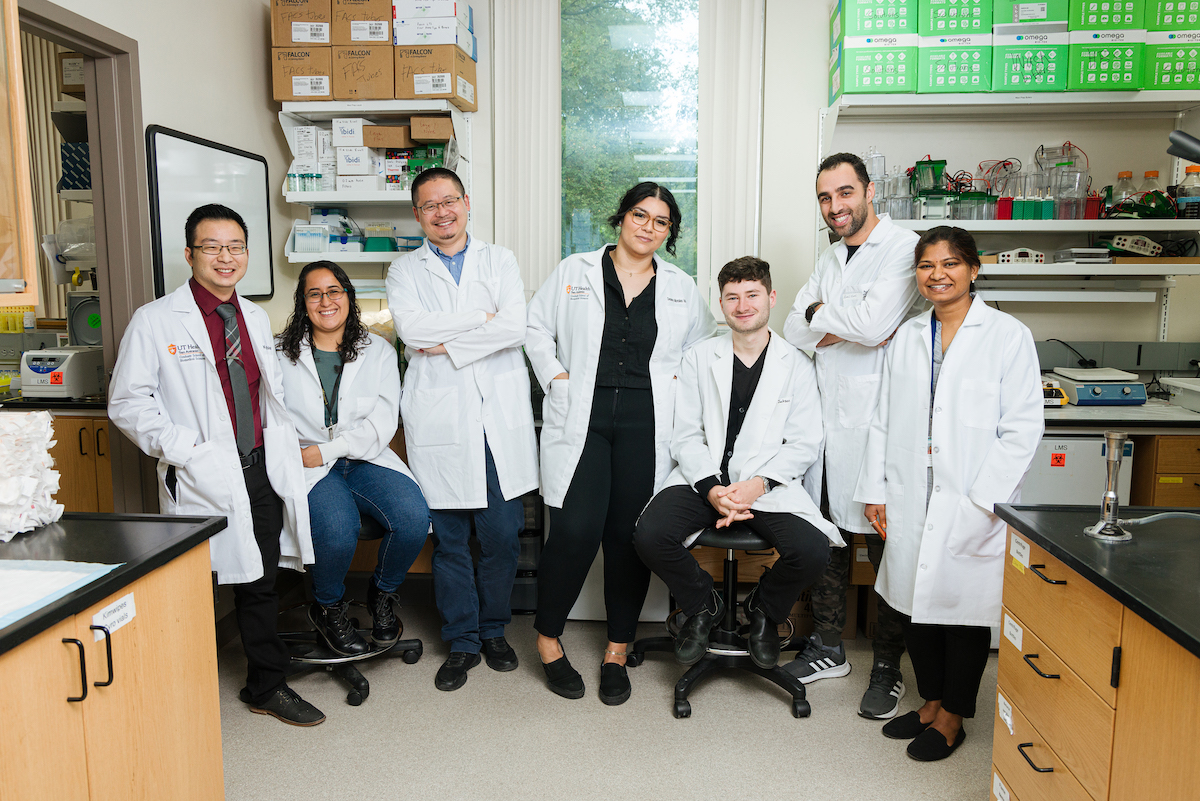
Because of Texas Biomed’s expertise in generating and using these critical reverse genetics tools, numerous national and international groups are now collaborators. For example, Dr. Martinez-Sobrido is an investigator in three of the nine Antiviral Drug Discovery (AViDD) Centers for Pathogens of Pandemic Concern. The National Institutes of Health (NIH) is funding these large centers to accelerate development of treatments for COVID-19 and other viruses that could cause future pandemics.
“We have to prepare for next time,” Dr. Martinez-Sobrido says. “By establishing the tools, methods and networks now, we will have the necessary systems and collaborations in place to respond faster to future outbreaks and a suite of antiviral medications at the ready.”
The viruses generated with the reverse genetics system in Dr. Martinez-Sobrido’s lab are playing a key role in screening those medications. For example, glowing reporter viruses help researchers quickly see if an antiviral drug is neutralizing the virus, or not. Essentially, no glowing means no virus and the treatment worked.
Speed has been everything in this pandemic.
“This is the fastest we’ve ever had to work,” Dr. Martinez-Sobrido says. “We weren’t done developing reverse genetics for one variant before the next one emerged. We had to prioritize and focus only on the dominant variants like Delta and Omicron.”
HOW REVERSE GENETICS WORKS

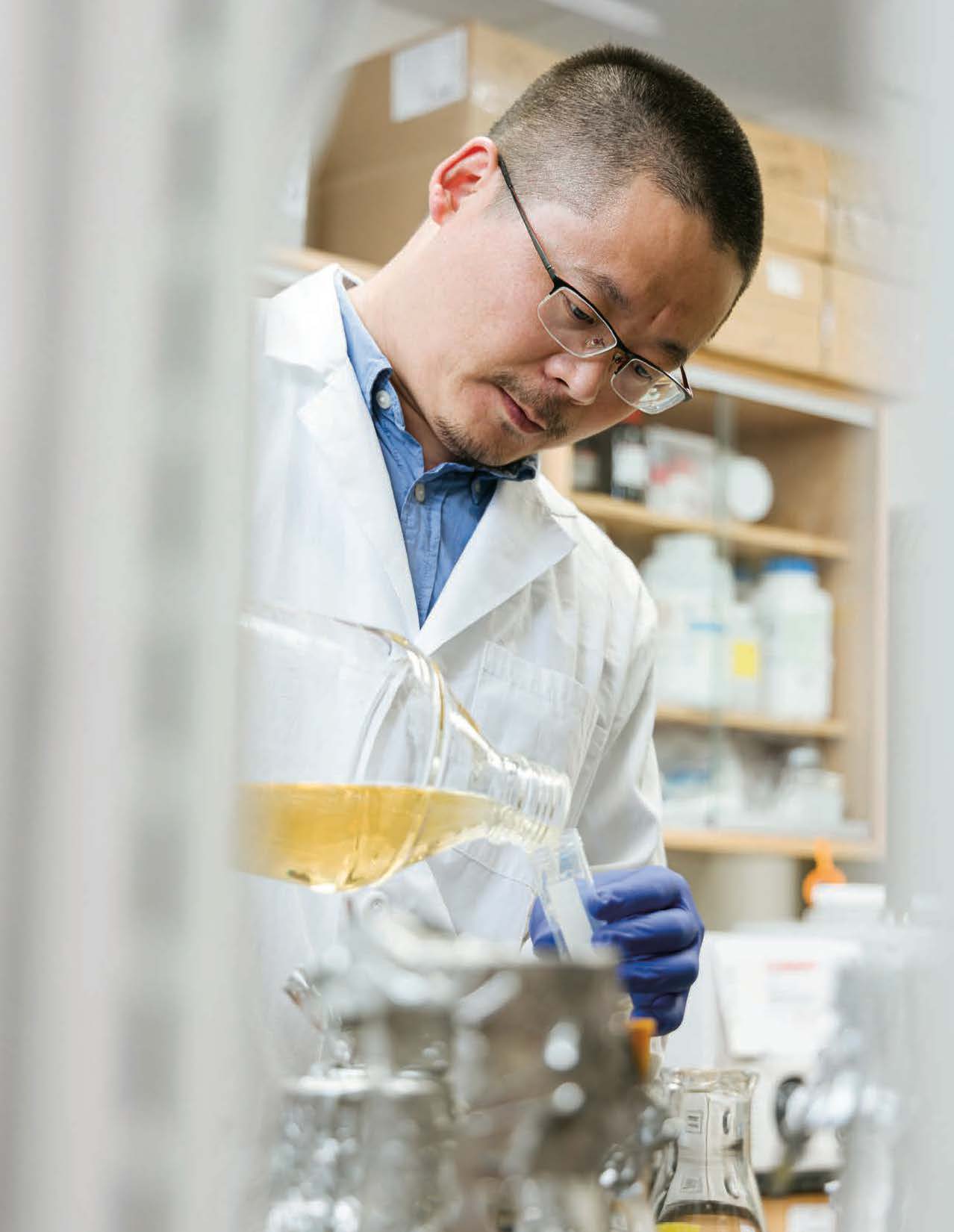
Dr. Ye inserts the first DNA fragment into the BAC, then puts the BAC into harmless bacteria cells in a petri dish. Once the bacteria clone themselves a few times, he carefully scoops out the tan blobs and runs genetic tests to confirm the bacteria contain the BAC with the fragment. Then, he must scaleup from a few BACs to a test tube full, in order to have enough material to work with. He places a few bacteria cells into a large flask filled with a golden liquid — yummy bacteria food — and leaves it on a shaking platform for 16 hours.
During the height of the pandemic, Dr. Ye would come back to the lab when the 16 hours were done to proceed to the next step, even if it was in the dead of night, the middle of the weekend or a holiday.
“There was not a minute to waste,” he says. “The whole team was working around the clock. We were trying to catch up with the virus.”
While moving the process along as quickly as possible, it still takes two to three weeks to complete. Dr. Ye must repeat all the steps for each of the five fragments— carefully checking his work along the way to ensure that, one by one, each fragment is added correctly to the BAC, until finally, he has a complete DNA sequence in the BAC.
VOILÁ, VIRUS
Up until now, all the work has been on DNA, which is noninfectious. Now, it is time to go into the more restrictive BSL-3, where a small amount of BAC is placed in petri dishes filled with one million mammalian cells. Once the BAC successfully enters the cells, the cells’ normal machinery begins to translate the DNA into RNA… voilá, now that’s the virus.
It was a Sunday morning in June 2020 when Kevin Chiem — a graduate student who had moved with the group from New York to Texas and will soon complete his doctoral degree —called Dr. Ye to tell him the cells in the petri dishes showed signs of infection.
Genetic tests confirmed the carefully prepared protocol had worked and they had “rescued” a recombined version of SARS-CoV-2. This recombinant SARS-CoV-2 was virtually identical to the original strain and behaved the same. The team published the work a few months later, noting it was the first time this had been done forSARS-CoV-2 using a BAC. They used the same approach to generate glowing reporter viruses, which they published in 2021.
Their system presents advantages to others; primarily, they use cells to transcribe DNA into RNA, rather than having to do this manually. Once cells make the first viral RNA copy, the RNA is translated into viral proteins and then itis off to the races. Not only are the cells helping the virus replicate, the viral particles are also replicating away.
“All we need is a little bit of BAC, and after this, we don’t have to do anything, they will help themselves,” Dr. Ye says.
All that virus — which is securely stored in the BSL-3 — can then be used to conduct experiments to understand how the virus works, and to evaluate vaccines and medicines.
For example, the generated viruses have since helped test the effectiveness of antiviral drugs, vaccine candidates and monoclonal antibodies, including a cocktail developed by Texas Biomed and the University of Alabama at Birmingham that Aridis Pharmaceuticals is working to advance to clinical trials. They have also helped develop animal models needed to study COVID-19.
The viruses have facilitated hundreds of studies at Texas Biomed and beyond. The BAC, which by itself is not infectious, has been shared with more than 100 groups with access to BSL-3 facilities. Dr. Ye has a -80ºC freezer full of BAC ready to ship as new requests come in.
“We have received requests every single week since we published the work in the scientific literature,” Dr. Martinez-Sobrido says.
MATTER OF MONTHS
With the main protocol established, researchers can now make specific changes to the DNA and test what happens, for example knocking out one or two genes. They pop out the original fragment from the BAC and pop in the edited version, like changing the ink cartridge in a printer.
That is how Dr. Martinez-Sobrido and his team were able to discover knocking out two genes resulted in an attenuated, or weakened, virus that does not cause illness nor death in two different animal models. They recently received approval from the NIH Office of Science Policy to work with this nonharmful strain in the BSL-2 — believed to be the first such approval in the U.S. — which will enable them to screen drug candidates even faster and safer.
“We can now try to answer important questions about the biology of the virus, which was not allowed before because of the risk involved,” Dr. Martinez- Sobrido says. “This attenuated virus enables us to do those types of studies safely.”
They are also exploring if it can work as a live attenuated vaccine. Live attenuated vaccines could provide longer-lasting protection and are used form any other viruses, including chickenpox, smallpox and polio.
“Historically, it took decades to discover attenuated strains that could work for vaccines,” Dr. Ye says. “With reverse genetics, we are able to do this in a matter of months.”
Key to all of this was the BSL-3 laboratory. Without it, the studies would not have been able to proceed safely. For Dr. Martinez-Sobrido, Dr. Ye and the team, moving to Texas Biomed to have access to a BSL-3 made all the difference.
“If we had not come to Texas Biomed, we would have been an audience to the pandemic,” Dr. Ye says. “While of course we wish there had not been a pandemic, we are glad we could make some important contributions to help get us to where we are today and to prepare for the next one.
Many of the molecular tools common in biology labs are for working with DNA. That is a challenge for virologists, because most viruses are made out of RNA. If researchers want to edit the virus’s genetic code, they have to first convert RNA into DNA, edit the DNA, and then transcribe it back into RNA.
Another challenge is the size of the SARS-CoV-2 genome. It is the biggest among RNA viruses; three times bigger than influenza and packaged in a single molecule. In order to work with it, researchers must cut up the genome, make several copies of the fragments, and then carefully reassemble the pieces.
Dr. Ye worked with an external company to do part of this process — obtaining the DNA sequences that correspond with the viral RNA genome. He designed the protocol for how the DNA sequences should be divided into five fragments and how to put them back together. The fragments have unique markers on either end so they can be reassembled in the correct order.
“The markers are essential,” Dr. Martinez-Sobrido says. “This is the only way that we can reassemble the virus.”
A small number of DNA fragments are shipped to Texas Biomed — since it is DNA, they are not infectious and can be handled safely in the biosafetylevel-2 (BSL-2) lab. To make lots of copies, a process called amplification, Dr. Ye turns to a virologist’s best friend: bacteria.
Bacteria are replicating machines, cloning themselves every 30 to 50 minutes. If you want to make a lot of DNA copies, bacteria are among your best bets.
“We trick the bacteria into making copies for us by using a bacterial artificial chromosome, or BAC for short,” Dr. Ye says. Think of BAC like a vehicle used to transport genetic information. It is a circular molecule that looks and behaves like a bacterial chromosome and is easy for bacteria cells to replicate.