Professor Luis Martinez-Sobrido, Ph.D., (left) and Staff Scientist Ahmed Mostafa Elsayed, Ph.D., (right) review test results for the presence of bird flu while wearing protective equipment required for biosafety level-3 laboratories.
Bird Flu: A race against evolution
Texas Biomed researchers are working on vaccines, antivirals and other therapies to protect people from highly pathogenic avian influenza viruses.
Ahmed Mostafa Elsayed, Ph.D., was in the lab when the news broke: highly pathogenic avian influenza was infecting dairy cows and a farmworker in Texas.
The headlines on April 1 caught his attention for two reasons: one, bird flu had never been detected in cows before; and two, he had just begun studying that strain of bird flu, H5N1, in a biosafety level-3 (BSL-3) lab at Texas Biomed.
“We had been working for a year to get all the approvals and licenses and had started our studies literally the week before,” recalls Dr. Elsayed, who is a Staff Scientist in the lab of Professor Luis Martinez-Sobrido, Ph.D.
That groundwork meant Texas Biomed was uniquely positioned to immediately respond to the unfolding outbreak, which caused initial concern about potential threats to human health, the nation’s milk supply and U.S. farm and cattle industries.
Dr. Martinez-Sobrido, an expert in influenza and other emerging viruses, quickly convened his team to discuss how the news would shift their H5N1 research plan. The scope of work – developing genetic-based tools and animal models and using those to evaluate the effectiveness of existing antivirals, antibodies and vaccines – remained the same. All they needed to do was add in the specific H5N1 strain from Texas and prioritize which questions to study first.
“We are thinking about what are the most important things that we need to do right now,” says Dr. Martinez-Sobrido. “Although there is not a concern of a pandemic yet, it is important to be prepared.”
THE CLOCK IS TICKING
That’s the good news: currently, H5N1 is not transmitted easily between people so the overall public health threat is low. However, since this H5N1 variant first emerged in Europe in 2020, it has spread rapidly through wild birds around the world and killed millions of chickens, which is why it is classified as “highly pathogenic avian influenza.” It was first detected in North America in late 2021, leading to multiple poultry outbreaks in 2022. Meanwhile, it has also spread to a wide variety of mammals – foxes, raccoons, skunks, opossums, mink, coyotes, mountain lions, black bears, grizzly bears, polar bears, seals, sea lions, cats, dogs – the list goes on. And now, for the first time ever recorded, cows.
Bird Flu Origins

Wild aquatic birds and waterfowl are natural reservoirs of avian influenza viruses, including gulls,ducks, terns, geese, swans and shorebirds.
- Detected in +100 wild bird species
- Typically, asymptomatic infection
“This is strange,” says Dr. Elsayed, who has studied avian influenza viruses for 16 years. “This virus can infect such a wide variety of hosts and it seems like every few weeks, it is showing up in a new species. That is why Dr. Martinez-Sobrido and I started talking in early 2023 that it would be important to study.”
Wild waterfowl and migratory birds are natural reservoirs for avian influenza viruses. Most do not typically get sick and the viruses evolve slowly in those birds. But when bird flu transmits to a new species, evolution speeds up. The viruses are working to adapt to their new hosts. Each time is a possible step closer to transforming into an upper respiratory infection that can be easily passed from person to person.
Since 1996, H5N1 has caused fewer than 900 human infections worldwide. Symptoms can range from mild to severe. The fatality rate has been high: more than 50 percent. As of publication, a few people in the U.S. have shown mild signs of infection and recovered, following interactions with infected farm animals.

Highly pathogenic avian influenza (HPAI) variants are so named because they are very deadly in chickens.
Avian influenza viruses are part of the same family of influenza A viruses that cause seasonal flu. However, influenza A viruses have a large number of different subtypes that the human immune system has never encountered. That is why avian flu has the potential to rapidly spread among people with no built-up defenses and potentially cause a pandemic.
“With a mortality rate of 50 percent – we would be talking about a different level of pandemic,” Dr. Elsayed says. “Right now, we are in low risk of pandemic, but to move to higher risk could happen in a matter of two or three weeks. We must be prepared.”
GETTING AHEAD OF THE VIRUS
To be able to study highly pathogenic avian influenza requires specialized, high-containment BSL-3 laboratories, as well as clearance from the Centers for Disease Control and Prevention (CDC) and U.S. Department of Agriculture (USDA) as part of the Federal Select Agent Program.
Texas Biomed applied to work on highly pathogenic avian influenza strains in 2023, receiving approval in the fall. Dr. Elsayed, working with Anthony Wang, Ph.D., Director of Texas Biomed’s Environmental Health and Safety, spent the better part of a year developing the required protocols, getting them approved and setting up the lab. After final review by regulators, he was ready to commence studies in March – a few weeks before the headlines hit.
The foresight and hard work positioned Texas Biomed as part of an elite group of labs with clearance to study H5N1 and other highly pathogenic variants.
“We can’t just start any time we want,” stresses Dr. Martinez-Sobrido. “We had to have the select agent BSL-3 laboratory set up, reviewed and approved. Now, we are on the front lines with our facilities to work on highly pathogenic avian influenza viruses.”
COORDINATED RESPONSE
Since H5N1 appeared in dairy cattle – and has since been detected in herds throughout the U.S. – Dr. Martinez-Sobrido and Dr. Elsayed have been on weekly calls at 7 a.m. with federal agencies and other scientists to discuss what different teams are working on and the latest updates. The calls are coordinated by the Centers of Excellence for Influenza Research and Response (CEIRR). Launched in 2021 by the National Institute of Allergy and Infectious Diseases, CEIRR is an international, multidisciplinary network of researchers studying key aspects of influenza and other pathogens with potential to cause pandemics.

Late March: First-ever
report of H5N1 occurring
in cows
“H5N1 is a clear example of how the network is helping share information quickly in response to an evolving situation and coordinate research efforts,” says Dr. Martinez-Sobrido.
He and his team did what they do best – getting to work on tools needed to study the virus and potential preventions and treatments. At the top of the list is evaluating existing antiviral medications to see if they work against this H5N1 variant.
“Antivirals are the first line of defense that we’re going to have if this virus starts circulating in humans and we have not been vaccinated,” Dr. Martinez-Sobrido says.

After suiting up in full-body suits,
head covers, boots, gloves and turning on their air-purifying respirators,
Dr. Elsayed and Dr. Martinez-Sobrido are ready to enter the BSL-3 lab.
Antivirals are the first line of defense that we’re going to have if this virus starts circulating in humans and we have not been vaccinated.
Dr. Luis Martinez-Sobrido
The team will also study, in collaboration with James Kobie, Ph.D., at the University of Alabama at Birmingham, if antibodies developed in their lab and existing vaccine candidates work against the virus. There is no approved bird flu vaccine, but the CDC has stockpiles of precursor materials – called candidate vaccine viruses (CVVs) – that could be manufactured into vaccines if the need arises. It appears two of those would provide protection against the current H5N1 variant if it were to begin spreading person-to-person.
“It would take time, unfortunately, to produce the vaccine and to have everybody vaccinated,” Dr. Martinez-Sobrido says. “Antivirals and antibodies could help treat people who become sick until vaccines are available.”
VIRUS EXPERTS
Dr. Martinez-Sobrido’s group is especially skilled at generating viruses in the lab using advanced techniques called reverse genetics. They use the synthesized viruses to test if treatments are effective and to ask key questions about how the virus works.
“There is a lot we do not know about this virus,” says Dr. Elsayed. “What makes it different from other avian influenza strains? How is it able to infect so many species? How does it spread?”
The team makes versions of the virus that glow, or fluoresce, so they can visually see if the virus is present or not in a sample. This saves a lot of time and resources when testing antivirals and antibodies – rather than having to run genetic-based tests to check if the virus is present in a sample, they can simply look to see if there are any glowing specs of virus.
They first study H5N1 in cells in Petri dishes. They are also developing protocols to study the virus in animal models.
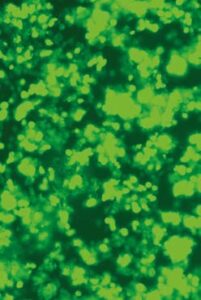
Researchers at Texas Biomed have developed glowing reporter H5N1 viruses to make it easy to visually spot the virus. Here, the green glowing spots indicate the virus is present. The researchers can use the reporter viruses when testing antivirals, antibodies or other treatments. If treatments are very effective, there should be no green specs left in the dish.
All of this is done in the safety of the select agent BSL-3. There are strict regulations on air flow, the handling of materials, disinfection procedures and who can access the lab. To enter, researchers must be fully suited up in a white Tyvek suit, head covers, shoe covers and two sets of gloves. They also wear a battery-powered air-purifying respirator that completely covers the head and face and filters particles out of the air. BSL-3 is the level of lab required to study pathogens that can spread through air, but that do not require the highest-level lab, BSL-4, because there are some treatments available. Pathogens commonly studied in BSL-3 labs include HIV, SARS-CoV-2 and the bacteria that causes tuberculosis.
WINDOW OF OPPORTUNITY
Thankfully, initial indications show existing candidate vaccines and antivirals will work against this H5N1. But influenza viruses are notorious for continuing to evolve – that’s why seasonal flu vaccines must be updated every year. Likewise, it is vital to develop an array of effective therapies and vaccines that can be readily adapted as bird flu shifts and changes.
“Our ultimate goal is a universal vaccine that can protect against many different influenza strains by targeting just the right section of the virus that cannot mutate,” Dr. Martinez-Sobrido says.
Many Mammals

H5N1 has spilled over sporadically into a wide range
of species, including foxes, raccoons, skunks, mink, bears,
mountain lions, seals, sea lions, otters, cats and dogs.
Without the legwork to get the facilities set up and the approvals and the clearance, Texas Biomed would not be in the position to contribute to these solutions. This requires sustained investment, which is always the challenge, notes Dr. Martinez-Sobrido. Often researchers are not funded to work on viruses with pandemic potential until there is an outbreak. That approach costs lives.
He pointed to the COVID-19 pandemic. Researchers knew a coronavirus could cause a pandemic, but funding to fully develop therapies and vaccines did not begin to flow freely until there was a public health emergency. While the vaccine rollout was the fastest in human history, it was still not fast enough. More than 3 million people had died before the first shots were given and the death toll has since eclipsed 7 million.
Bird flu is a reminder that we can’t get complacent. It’s also a chance – a window of opportunity – to do it differently and actually be prepared.
Makings of a flu shot
Candidate vaccine viruses (CVVs) are versions of influenza viruses that manufacturers then use to produce flu vaccines. The Centers for Disease Control and Prevention (CDC) and its partners routinely develop CVVs for seasonal flu shots, as well as for a variety of bird and swine flus that have pandemic potential. Texas Biomed is working with the CDC to generate CVVs, including for H5N1 bird flu. Generating CVVs is a complex process that must follow strict protocols since the material can ultimately end up as part of vaccines given to people. The process is even more challenging for highly pathogenic avian influenzas like H5N1. Researchers must synthesize versions of the virus that are far milder than the original, to the point they no longer cause severe illness or death in chickens, while stimulating an effective immune response in people. CVVs are thoroughly tested to ensure they are safe and effective against the targeted strains. The CDC distributes CVVs to vaccine manufacturers for additional testing and possible vaccine production to prepare for potential outbreaks or pandemics.
Funding information: Research on influenza in Dr. Martinez-Sobrido’s laboratory is currently funded by the Centers of Excellence for Influenza Research and Response, the American Lung Association, National Institutes of Health grant R01AI145332 and support from Texas Biomedical Research Institute.